Diabetes is more than just a number on your blood sugar test. It’s a chronic condition affecting millions, turning the simple act of enjoying a meal into a complex balancing act of glucose management. Understanding it starts with recognizing it as more than what a blood test can show.
Knowing the difference between Type 1 and Type 2 diabetes is crucial. Why? Because it directs how individuals manage their health daily. It’s easy to lump them together as they both revolve around high blood sugar levels, but the routes they take to get there can’t be more different. Recognizing these differences isn’t just for those diagnosed, yet it’s a step towards empathy and better support systems for everyone.
The purpose of this article is straightforward: I aim to clear up the confusion. By laying out the distinctions between Type 1 and Type 2 diabetes, I’ll guide you through what each means, how they manifest, and why it matters. Whether you’re living with diabetes or you know someone who is, having a clearer picture helps in navigating life smarter and healthier.
Decoding Diabetes: Understanding the Basics
Let’s break down diabetes, a key player in metabolic disorders. It’s a condition where the body’s ability to process glucose, a simple sugar vital for energy, is disrupted. In simpler terms, diabetes messes with how your body deals with sugar, which can leave your blood sugar levels out of whack.
Central to this problem is insulin, a hormone produced by the pancreas. Insulin acts like a key, unlocking cells to allow glucose from your bloodstream to enter and be used for energy. When insulin’s role doesn’t play out right, glucose builds up in the blood instead of doing its job fueling your body.
There are a couple of main scenarios where things can go wrong: either your body isn’t making enough insulin, or it isn’t using it well. That’s where you get the different types of diabetes – Type 1 often involves little to no insulin production, while Type 2 typically sees the body struggling to use insulin effectively.
Understanding how glucose and insulin interact is fundamental. This understanding forms the backbone of managing diabetes, guiding everything from medication to meal planning. It’s not just knowing what diabetes is – it’s about grasping the ‘why’ and ‘how’ so you can tackle it head-on.
Type 1 Diabetes: An Autoimmune Puzzle
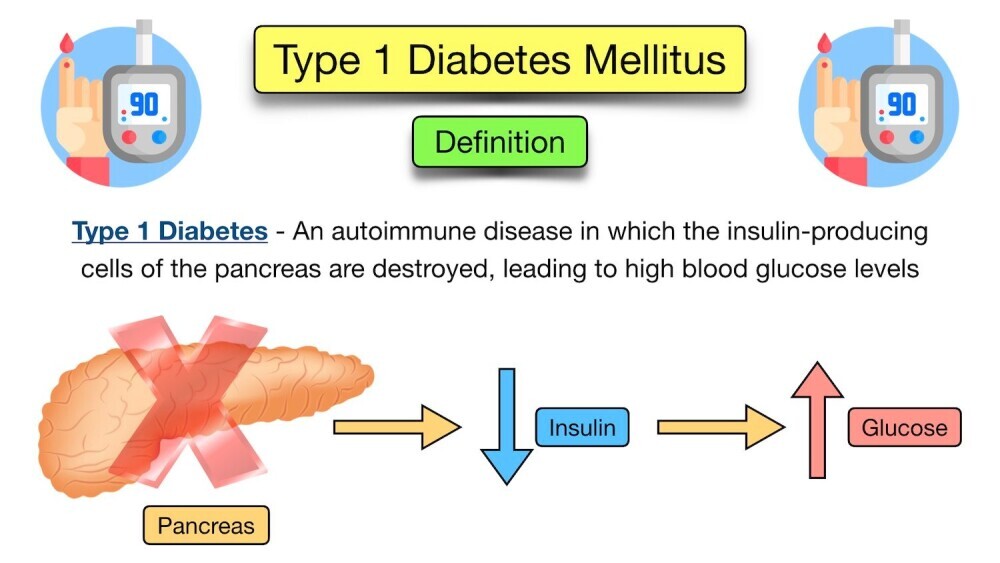
Type 1 diabetes steps into the spotlight as an autoimmune condition, where the body’s defense system gets its wires crossed. It mistakenly attacks insulin-producing beta cells in the pancreas. This isn’t a problem of poor lifestyle choices, but rather a situation where the immune system turns against itself.
Typically diagnosed in the younger crowd—kids and young adults—Type 1 diabetes often shows up unexpectedly. One moment, life is rolling along smoothly, and the next, symptoms like thirst, frequent urination, and unexplained weight loss become part of the daily routine. It’s not just a phase; it’s an urgent call to action.
Managing Type 1 diabetes requires some lifestyle alterations and a commitment to constant monitoring. Insulin therapy becomes a daily companion, balancing blood sugar levels to mimic what the body would naturally do. Diligent blood glucose monitoring, coupled with mindful eating and exercise, forms the cornerstone of managing this condition.
While living with Type 1 diabetes involves a learning curve, having the right information sets the foundation for effective management. It’s about knowing what to expect and having the tools to manage it efficiently. With a proactive approach, those diagnosed can lead full and active lives, equipped with strategies to tackle each day head-on.
Type 2 Diabetes: A Growing Concern
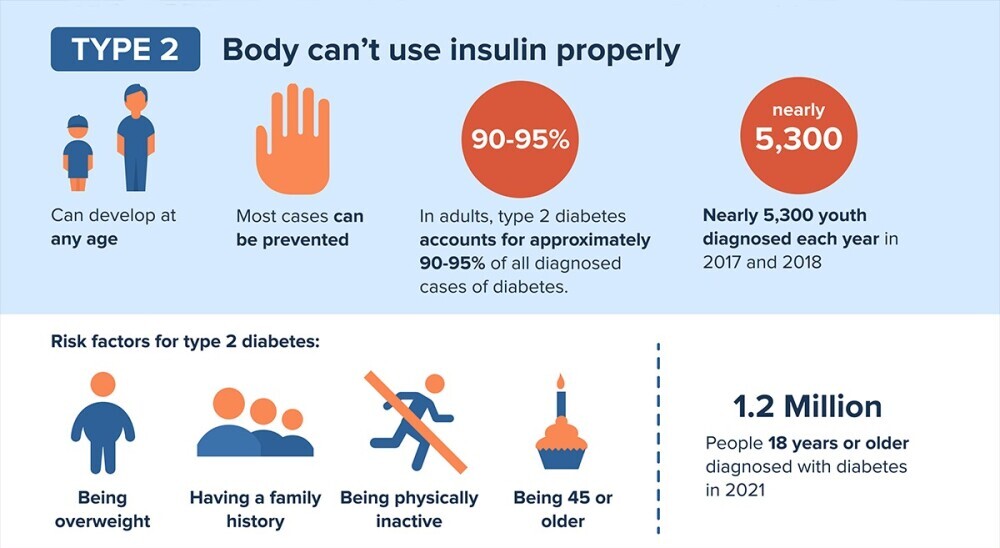
Type 2 diabetes has garnered attention not as a silent invader but as a condition linked closely with our contemporary lifestyles. It stems from the body’s struggle to use insulin efficiently, leading to insulin resistance, and gradually the pancreas may reduce insulin production. In simpler terms, the body becomes less responsive to the insulin available, making it harder to manage blood sugar levels.
Risk factors don’t just appear overnight. Obesity, a sedentary lifestyle, a family history of the disease, and age are major contributors. What’s notable is the shifting age demographic with more children diagnosed, echoing changes in lifestyle and diet across generations.
Symptoms may mimic those of Type 1—intense thirst, frequent bathroom breaks, fatigue—but often develop slowly. This gradual creep can make it harder for some to recognize early signs that require medical attention. It’s not uncommon for people to be diagnosed in routine check-ups, having adapted unknowingly to early symptoms.
Management is a multi-faceted approach. Watching what goes onto your plate, committing to regular physical activity, and sometimes employing medication—either oral or injectable—form the crux of maintaining well-balanced blood sugar levels. Monitoring remains key; keeping those glucose levels in check is crucial to mitigate long-term complications.
Understanding Type 2 diabetes involves recognizing the role lifestyle changes play in prevention and management. Regular health evaluations and lifestyle modifications not only help in managing the condition but can also prevent its onset in those predisposed. Emphasizing these adjustments can greatly enhance quality of life.
Discerning Differences: Type 1 vs. Type 2 Diabetes
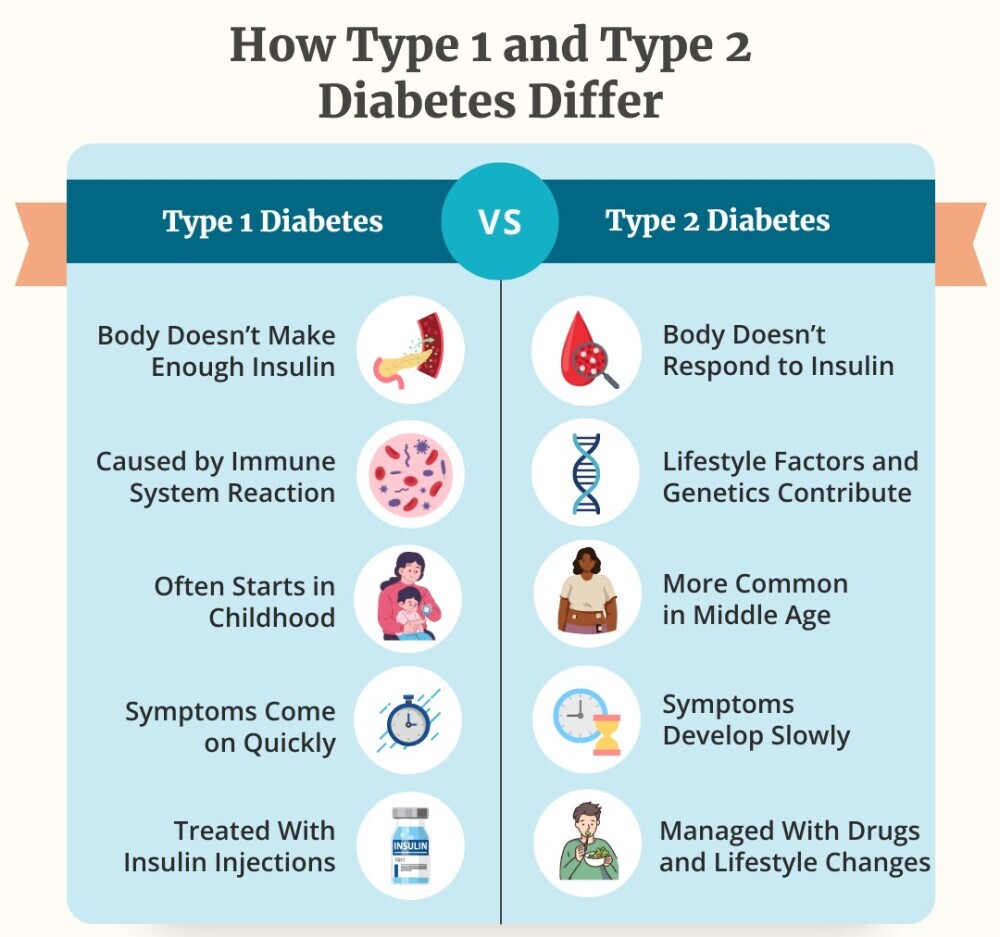
Understanding the fundamental distinctions between Type 1 and Type 2 diabetes clarifies why their management strategies differ so much. Each type travels its unique path, impacting lives in diverse ways.
Type 1 diabetes kicks off because of an autoimmune response, where the body mistakenly targets its own insulin-producing cells. This rapid onset can occur suddenly, often without much warning, particularly among the young.
In contrast, Type 2 diabetes unfolds more stealthily. It is predominantly influenced by lifestyle and genetic factors, blooming slowly often over many years. Here, the body builds up a resistance to insulin, leading to an eventual reduction in insulin levels over time.
When it comes to insulin dependence, here’s the distinction: individuals with Type 1 diabetes require lifelong insulin therapy, which becomes an essential part of daily life. However, those with Type 2 may manage without it initially, also relying on lifestyle changes and other medications to control their blood sugar levels.
Prevalence paints a stark picture: Type 2 diabetes is far more common than Type 1, reflecting its strong ties to lifestyle factors prevalent in today’s society.
Symptoms can blur the lines between the two types in their early stages. Both include increased thirst and fatigue, but Type 1’s onset is acutely rapid, whereas Type 2’s gradual development can leave symptoms unnoticed for longer periods.
This understanding enables more personalized management approaches, empowering individuals to tackle diabetes with strategies tailored to the specific type they are dealing with. Recognizing these distinctions helps in not just medical management, but also in fostering a deeper understanding of how diabetes affects different individuals.
Common Misconceptions Surrounding Diabetes
Misunderstandings about diabetes often cloud the real issues at hand, making management more challenging for those directly affected. A prevalent myth is that Type 2 diabetes always requires insulin therapy, parallel to Type 1. The truth is, Type 2 can often be managed with lifestyle interventions and oral medications, and insulin is introduced only if other methods fall short.
There’s also confusion over what causes each type. Many presume a poor diet is responsible for both, but it’s crucial to know that Type 1 has an autoimmune trigger unrelated to lifestyle. Meanwhile, Type 2 does have stronger ties to lifestyle habits and genetics.
Further complications arise from symptoms, which many believe are always noticeable. In reality, Type 2 symptoms develop gradually, often going unnoticed until health checks reveal the condition.
The misunderstanding extends to what constitutes a proper diet. People assume eliminating sugar solves the issue, overlooking the importance of a balanced diet focusing on whole foods, proteins, and fibers.
Clearing these misconceptions is vital as it affects how individuals seek treatment and manage their conditions. Accurate knowledge paves the way for effective management strategies and helps in reducing stigma, leading to better support systems within communities. Understanding these nuances position readers better to empathize and support those with diabetes.
Unveiling Risk Factors and Preventative Strategies
Type 1 diabetes, with its autoimmune roots, often stems from a genetic predisposition, but the role of environmental triggers can’t be entirely ruled out yet. There’s no prevention strategy currently available, leaving a focus on early detection and management as the primary defense.
Type 2 diabetes, however, opens the door for more proactive measures. Managing weight through a balanced diet and regular physical activity stands at the forefront of prevention. These aren’t just recommendations; they’re actionable steps that can significantly reduce the risk for those predisposed.
A balanced diet rich in whole grains, fresh vegetables, lean proteins, and healthy fats helps maintain a healthy weight and stable blood sugar levels. It’s not about a drastic overhaul but gradual, sustainable changes that fit individual lifestyles. Incorporating these habits can transform how the body handles glucose, lowering blood sugar levels and improving overall health.
Regular exercise complements dietary measures, enhancing insulin sensitivity and supporting weight management. It’s about finding activities that are enjoyable and sustainable, whether it’s walking, swimming, or cycling, and making them a regular part of life.
For those at risk, understanding these strategies isn’t just beneficial; it’s crucial. Knowledge empowers individuals to craft a lifestyle that not only combats Type 2 diabetes but also enriches their overall well-being. By embracing these changes, you can take a stand against Type 2 diabetes, minimizing its impact or preventing it altogether.
Timing is Crucial: Early Diagnosis and Treatment Imperatives
Diabetes can quietly lead to severe complications if left unchecked, underscoring the importance of early diagnosis and treatment. Complications like neuropathy, or nerve damage, along with increased risks for cardiovascular diseases, can sneak up on individuals over time. These aren’t just medical terms; they’re serious conditions that can significantly impact quality of life.
Timely intervention plays a pivotal role in managing and mitigating these risks. By spotting the signs early and seeking medical advice, individuals can navigate their diagnosis with a clear strategy. Early treatments often involve lifestyle changes and medications that help maintain blood sugar levels within a healthy range, averting more severe health issues down the road.
The benefits of early diagnosis extend beyond health metrics. It offers the opportunity to educate oneself about the condition, allowing for comprehensive management plans tailored to individual needs. Understanding the potential impact and taking empowered steps toward management encourages not just better health outcomes but also fosters a sense of control over one’s life.
Regular health check-ups are a key component in this strategy. They provide essential insights into how well-management efforts work and adjust plans as needed. This proactive approach ensures long-term health stability and can dramatically enhance life quality.
Choosing to pursue early diagnosis and treatment isn’t merely a reactive measure; it’s about utilizing available knowledge and tools to take charge of one’s health journey. Engaging with healthcare professionals and leveraging their expertise is invaluable, setting a foundation for a healthier future amidst the challenges diabetes might bring.
Navigating Life with Diabetes: Support and Resources

Living with diabetes involves not just medical management but also navigating the psychosocial landscape it brings. It’s a journey that requires both physical and emotional resilience, accompanied by continuous learning and adaptation.
Key tools like glucometers and insulin delivery systems help manage blood sugar levels effectively, turning potential challenges into manageable tasks. Education plays a significant role in understanding how various factors affect blood sugar levels, from food to stress.
Support systems, including family, friends, and medical professionals, provide invaluable guidance. Their role extends beyond just emotional support; they offer practical advice and help build frameworks for long-term management strategies. Being surrounded by a supportive network makes navigating daily challenges less daunting.
Communities, both online and offline, offer spaces to share experiences and advice. Engaging with others who understand the intricacies of diabetes can be empowering. These interactions breed a sense of camaraderie and understanding, alleviating feelings of isolation.
Access to educational resources, such as workshops and informational websites, empowers individuals to stay informed about the latest diabetes management strategies. Keeping abreast of new research and technological advancements can optimize how one lives with diabetes.
Taking an active role in one’s diabetes management journey ensures not only better control over the condition but also improves quality of life. Emphasizing education, community, and proactive health management equips individuals with the tools needed to handle whatever comes their way.
Conclusion
Diabetes is more than a clinical diagnosis or a series of numbers on a blood test. It’s a condition that reshapes daily life, demanding a deeper understanding of how the body processes energy and the pivotal role of insulin. Recognizing the key differences between Type 1 and Type 2 diabetes is not just about knowing their definitions—it’s about understanding their unique challenges and how they shape individual lives.
Type 1 diabetes arises from an autoimmune reaction, often striking without warning and requiring lifelong insulin therapy. On the other hand, Type 2 diabetes develops gradually, influenced by lifestyle factors and genetics, with management focusing on prevention, diet, exercise, and medications. While their symptoms and impacts may overlap, their underlying mechanisms and management strategies differ greatly.
By distinguishing between these two types, we not only foster greater empathy and support for those living with diabetes but also empower individuals to take control of their health. Early diagnosis, informed choices, and proactive management are crucial for navigating life with diabetes effectively.
Understanding diabetes goes beyond medical facts—it’s about embracing a holistic approach to health and equipping ourselves to support those affected. Whether you’re living with diabetes, know someone who is, or simply want to learn more, knowledge is the first step toward healthier and more informed lives.
** Our website contains affiliate links. This means if you click and make a purchase, we may receive a small commission. Don’t worry, there’s no extra cost to you. It’s a simple way you can support our mission to bring you quality content.
FAQ
What are the main differences in treating Type 1 and Type 2 diabetes?
Type 1 Diabetes Treatment:
Requires lifelong insulin therapy since the body cannot produce insulin.
Includes frequent blood sugar monitoring and the use of insulin pumps or injections.
Requires careful carbohydrate counting and dietary management.
Type 2 Diabetes Treatment:
Often starts with lifestyle changes, such as adopting a healthy diet, regular exercise, and weight management.
May include oral medications or injectable drugs like GLP-1 receptor agonists.
Some individuals may eventually require insulin therapy if other treatments are insufficient.
How can doctors tell the difference between Type 1 and Type 2 diabetes?
Doctors differentiate the types using:
1.Age of Onset: Type 1 often occurs in children or young adults, while Type 2 is more common in adults but can occur in children.
2.Blood Tests:
- C-peptide test: Low levels suggest Type 1 diabetes (minimal insulin production).
- Autoantibody tests: Presence of antibodies indicates Type 1 diabetes.
3.Symptoms and History: Rapid onset of symptoms (Type 1) versus gradual onset (Type 2).
4.Physical Characteristics: Type 2 is often associated with obesity or metabolic syndrome, while Type 1 is not.
How to differentiate between Type 1 and Type 2 diabetes in children?
Type 1 Diabetes in Children:
- Often presents with sudden symptoms like excessive thirst, frequent urination, unintended weight loss, and fatigue.
- Diagnosed through autoantibody tests and low C-peptide levels.
- Typically requires immediate insulin therapy.
Type 2 Diabetes in Children:
- Symptoms develop gradually and may include darkened skin patches (acanthosis nigricans) and mild fatigue.
- More likely in children with obesity and a family history of diabetes.
- Diagnosed based on C-peptide levels (higher than in Type 1) and the absence of autoantibodies.
What are the differences between Type 1 and Type 2 diabetes, including risk factors for each?
Type 1 Diabetes:
- Cause: Autoimmune destruction of insulin-producing beta cells.
- Risk Factors: Genetic predisposition, family history, and possible environmental triggers like viruses.
- Age of Onset: Usually diagnosed before age 30.
Type 2 Diabetes:
- Cause: Insulin resistance and eventual decline in insulin production.
- Risk Factors:
- Obesity and sedentary lifestyle.
- Family history of Type 2 diabetes.
- Age (more common after 40 but increasingly seen in youth).
- Certain ethnic groups (e.g., African American, Hispanic, Native American).
What is a key difference between Type 1 diabetes and Type 2 diabetes?
The key difference lies in the cause:
- Type 1 diabetes results from the body’s immune system attacking insulin-producing cells, leading to little or no insulin production.
- Type 2 diabetes arises from insulin resistance, where the body does not use insulin effectively, often accompanied by decreased insulin production over time.
What is the difference between Type 1 and Type 2 diabetes lifestyle?
Type 1 Diabetes Lifestyle:
- Requires consistent blood sugar monitoring and insulin administration.
- Individuals must plan meals, physical activities, and insulin doses carefully to maintain glucose levels.
- Diet is focused on managing carbohydrate intake without complete restrictions.
Type 2 Diabetes Lifestyle:
- Emphasizes weight management, healthy eating, and regular exercise to improve insulin sensitivity.
- Dietary focus includes low-glycemic foods, portion control, and reducing processed sugars and fats.
- Lifestyle changes can often delay or prevent the need for medication.
Some great informative information there. It took me many years to understand the changes in lifestyle and habits that have helped me lower my medicine intake and hopefully live normaly with type 2 diabetes.
Great information
Hi Kieran,
Thank you so much for your comment and for sharing your experience! It’s inspiring to hear how lifestyle and habit changes have helped you manage Type 2 diabetes and even reduce your reliance on medication. That’s such an important part of living well with diabetes, and your journey is a testament to the positive impact of consistent effort and awareness.
I’m glad you found the information in the article helpful. It’s always encouraging to hear from readers who can connect with the content on a personal level. Wishing you continued success and good health on your journey! If there are any specific topics you’d like to see covered in future articles, feel free to share. 😊
Cheers
John
Hi John
I found your article incredibly insightful and well-researched.
While I don’t have direct experience living with diabetes, I’ve seen the impact it has on others, including friends and colleagues.
Your explanation of the key differences between Type 1 and Type 2 diabetes helped clarify many misconceptions I had about the condition.
One thing that stood out to me was how important early diagnosis is in both types, especially when it comes to preventing complications.
It made me reflect on the value of regular check-ups for everyone, even those without symptoms, since early detection can make such a difference in long-term health outcomes.
I also appreciate how you highlighted the role of support systems, from family to online communities.
I’ve seen how these can be a game-changer for people dealing with chronic conditions—not just for emotional support but also for practical tips and shared experiences.
Your section on lifestyle changes for managing Type 2 diabetes was particularly eye-opening.
It’s inspiring to see how diet, exercise, and small, sustainable changes can have such a significant impact. It got me thinking about how we can all incorporate these habits into our lives, regardless of whether we have diabetes, to support overall health and well-being.
A couple of questions came to mind while reading:
How do individuals with Type 1 diabetes balance the need for constant insulin therapy with the unpredictability of daily life, such as exercise, stress, or illness?
For Type 2 diabetes, do you think workplace wellness programs or community initiatives focused on healthy lifestyles could play a significant role in prevention?
Thank you for shedding light on this important topic and providing such practical insights.
It’s a reminder of how much knowledge and proactive care can empower those living with diabetes to lead full and healthy lives.
Hi Raymond,
Thank you so much for your thoughtful comments and questions!
I’m glad you found the article helpful in clarifying the differences between Type 1 and Type 2 diabetes. To answer your first question, individuals with Type 1 diabetes often need to carefully balance insulin therapy with daily activities by closely monitoring their blood sugar levels, adjusting their insulin doses for exercise, and being mindful of how stress or illness can affect their glucose levels.
It can be a challenge, but with proper planning, support from healthcare providers, and a strong understanding of their body’s needs, many people with Type 1 diabetes manage these fluctuations effectively. Regarding Type 2 diabetes, I absolutely agree that workplace wellness programs and community initiatives can be game-changers. Promoting healthy eating, regular physical activity, and stress management in these settings can not only help prevent Type 2 diabetes but also create a supportive environment for those already managing the condition.
When these programs focus on education and lifestyle changes, they can foster a culture of prevention and long-term well-being. Your reflections on proactive care and lifestyle changes are spot on—small, consistent changes can have a powerful impact, and it’s encouraging to see how we can all benefit from these habits, whether or not we have diabetes.
Cheers
John